The programme aims to assist treating depression and anxieties that are directly related to the disease.
The Clinical Research Unit for Anxiety and Depression (CRUfAD), which is part of St Vincent Hospital’s mental health services, was key in iAdapt’s development. It is expected the confidential course will be available to the general public in mid-2018.
Dr Michael Millard, a researcher on the project, was able to answer some questions about the programme.
Can you explain more about the programme? We know that it is online, but what are some more specific things to expect from it?
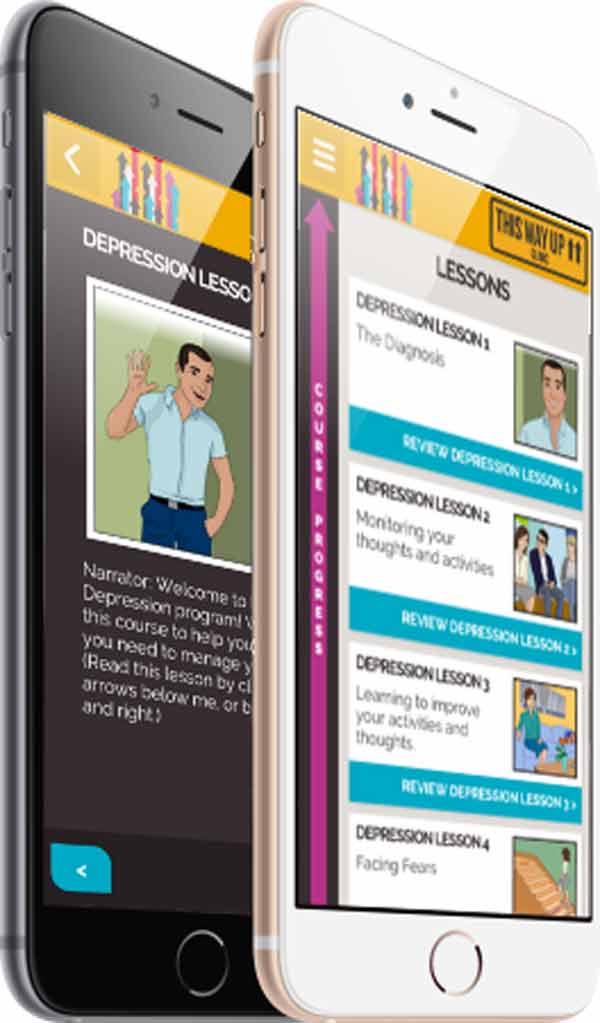
iAdapt is a new online confidential therapy programme which we specifically created for gay men who are living with HIV and might be struggling with emotional distress, anxiety or depression. The course draws on some of the fundamental processes we use to treat mental health issues and reintroduces it in an easy to navigate, accessible format – empowering people by teaching them practical, proven skills to self-manage their wellbeing. It equips them with lots of the skills we know to be effective and lasting. The beauty of the programme is its simplicity; it takes the form of an illustrated story of two characters who are living with HIV, by following their journey we learn about destructive cycles, the power of recognising those cycles and how to break them. It’s really an at-your-own-pace, self-directed programme that offers supportive guides and many other useful resources; from tips on sleep and mindfulness – through to advice for family, friends and others in people’s support networks. Each week of the programme a new lesson is unlocked allowing people to practice and apply the skills to their own life at a steady pace and not become overwhelmed with information. Additionally, during the evaluation trial all patients in the programme are supervised by a psychologist or medical doctor ensuring close monitoring of distress levels and patient safety. Striking the balance of unobtrusiveness and high level care has been important in creating a safe, trusted environment for our participants.
What is your involvement with the programme?
I’ve been involved from the beginning. I am currently the research fellow in mental health at Sydney’s St Vincent’s Hospital. In my position as a medical doctor who specialises in mental health, I have a keen interest in the interrelationship between physical and mental health so the combination of a chronic illness and its impact on our mental wellbeing is central to my work. Prior to moving into mental health I trained in General Practice including HIV in inner Sydney, every day I was witnessing the need for a programme that could offer a solution to a problem that many GPs were ill equipped to deal with – not by training by due to time constraints and workload. In developing iAdapt, this opportunity has allowed me to work closely with the community and local clinicians to develop content that delivers tailored, practical solutions, with the potential to now reach far beyond this community.

Was there a particular reason that you decided this is a much-needed service?
We already know that the LGBT+ community experience depression at a rate three times higher than the general population and are at least two times more likely to experience anxiety. We also know that almost 90 per cent of people living with HIV in Australia are men who have sex with men. Of that figure over 40 per cent report to experience significant depression. What is becoming alarmingly apparent is that very few of these men are receiving adequate treatment and there are multiple barriers that exist to accessing even basic effective care.
What kind of research was involved to get this all started?
We started by having a look at what options were out there for people already, and we found that there were really no tailored treatments for anxiety and depression for gay men who are living with HIV. From there we isolated what the most beneficial skills and tools would be for this kind of treatment and we allowed that to form the framework for the programme. The use of illustration and storytelling was decided upon as an easy to digest, relatable mode of treatment. Studies have shown us that internet-based treatment can be just as successful as face-to-face treatment.
How did it all come together?
St Vincent’s hospital has established itself as a world leader in both mental health and treatment of HIV. Having been at the forefront of best practice treatment for HIV right from the start of the epidemic, it’s a phenomenal achievement that with the medical advances over the last three decades, HIV is now a manageable chronic disease with a life expectancy nearing the general population. And that now shifts our focus to how we can best support those living with the chronic disease and foster their wellbeing. At the Clinical Research Unit for Anxiety and Depression we’ve had over thirty years’ experience in treating anxiety and depression in the general population with ten of those more recently demonstrating the successes to be had with online treatment options. Our previous research has shown that 80% of people who do our courses benefit from them and over 50% would no longer be classified as clinically depressed. We believed that to combine these two strengths would produce something very worthwhile.

Were there any challenges in getting it moving?
We certainly struggled with funding which has been disappointing. That’s been our biggest limitation. The patients, clinicians and the community jumped right aboard. We would love to see more support from the private and public sectors. The potential for this programme is huge.
Is it recommended that the programme be used in conjunction with other specialists, such as a psychiatrist or counsellor? Or will iAdapt incorporate this to some extent?
I see iAdapt used in a variety of different ways. In my own practice I’ll certainly be using it as an additional tool alongside face-to-face therapy for my patients. The online format means you can use it at home or on the bus in your own time and then in the face-to-face sessions I can focus on applying the skills or specific stressors. One of the great things is that the system also uses tools to track patient wellbeing and will send through an alert (to the clinician) if it picks up that someone is struggling or may need more help. I’ll certainly be encouraging other clinicians (of every variety) to use this alongside their traditional practice. On the other hand the iAdapt programme can ably stand alone as that important first step in someone accessing good evidenced based care online.
What do you hope will be the outcome of iAdapt?
At the end of the day, I hope that iAdapt is able to help people increase their wellbeing and get out and live their lives to the fullest. The tragedy of chronic disease and mental health is that a lot of people live with a sense of isolation and helplessness, it is our hope that this can restore some autonomy and resilience to people who feel sidelined by society on account of their condition. We’d also like take what we are learning from iAdapt and develop similar tailored interventions, the potential is boundless – from women with HIV, our indigenous population and so on. The model is sound and as the practices are proven to be effective it would be fantastic to see where else this method of treatment and care giving can be applied.
There has been a trial of the programme, what are the participants saying about it?
The feedback has been overwhelmingly positive. Participants tell us that have found it very easy to identify with one or other of the characters and follow the lesson programme at their own pace. It includes a wide range of skills – and there is plenty within the lessons to explore and practice wellbeing. We’re still open for applicants to join the programme too. So if you or someone you know might be interested we encourage you to apply at adapthiv.org.au – even though we are in Darlinghurst you don’t need to be in Sydney.
Should iAdapt prove successful, and that it is a world-first treatment specifically for men with HIV, do you hope the course will make its way into other countries?
Absolutely! We’re firmly of the belief that this is a treatment that has global potential. We’d be thrilled to see it rolled out wherever there is need.
iAdapt is expected to become available to the general public in mid-2018.






